Since the 1996 edition of Eating Right 4 Your Type by Peter J. d’Adamo, there have been many publications suggesting that one can modify his or her diet based on blood type for a number of benefits. Supposedly, a close adherent to a diet determined by blood type (A, B, AB, and O) can prevent or reduce the effects of allergies, arthritis, cancer, and aging—and of course, easily lose weight. Is this approach grounded in observable science? How likely are the dietary recommendations from the blood type diet (BTD) to improve your health?
Introduction: How to Read this Article
I have been interested in this topic for quite some time, so I’ve chosen to go with the long form on this one. In the interest of digestibility, I have sectioned it out so that you don’t have to read the entire article. If you get to a part you don’t find interesting, skip it—I don’t care. This article is for me as much as for you.
I have run into a lot of people in the health and wellness community that swear by the blood type diet (BTD). They follow it closely and have seen some dynamic improvements to their lives. I had a negative bias going into this, because I guess I’ve read too many organic chemistry books. And I’m stuffy. However, my goal here is to put my bias aside, dig deep into the topic and give it some critical thought.
In contract law, there is something called severability, which is used when one part of the contract is invalidated and the rest of the contract is upheld. Is this a valid mindset when researching health and wellness? What constitutes a fatal flaw from which the theory cannot recover? Can we dismiss certain elements of the blood type diet while we keep the good parts? Ultimately, that is up to you to decide. There are people out there who might find a typo on page 43 and stop reading, where others would keep going. I would encourage you, regardless of your prior conception about it, that you maintain a healthy curiosity. You might learn something, or you might uncover a mistake I have made and teach me something.
This critical review reflects some discrepancies found between the blood type diet and the scientific consensus. If you’re a “believer” in the diet, this might turn you off. But I recommend that you instead look past your convictions and continue reading to increase your understanding of the human body and how it works. Further, I would hope that the blood-type dieter would want to find any way to refine and improve the blood type diet. I can assure you there’s something in here for everyone, regardless of their prior knowledge on the subject.
Using Genetic Function to Individualize Diet
The blood-type diet (including d’Adamo’s adaptation and any subsequent or previous version of it) was one of the first diets to use reliable, biological tests to customize nutrition based on the needs of the individual. Its contemporary diets gave the same nutritional prescription to everyone. The Vegetarian Society dates to 18471. Their diet was refined by the vegans, who took out milk, eggs, and honey. Then there was the low-fat craze of the 1980s, followed by the Atkins diet a decade later, where the Atkins told people to eat more fat and less carbohydrates.
You probably know at least one person who swears by one of these diets, but plenty of other people who have tried them and had a bad experience. So, how do we determine the validity of each diet’s benefit? That’s where the study of evolutionary biology comes in. Scientists look at genetic traits and the evolutionary pressures that allowed them to become advantageous, then determine how they are harmful or helpful for us today.
The Basics of Evolutionary Biology
Let’s look at the famous example of sickle cell anemia. Most mainstream scientists believe in the malaria hypothesis. This theory was founded by scientists who noticed that sickle cell anemia was more common in tropical parts of the world. Some originally thought that the high temperatures were causing the red blood cells to change shape, but as technology progressed, it was discovered that sickle cell anemia was a genetic condition, meaning that people are born with it.
So why is sickle cell anemia more common in tropical regions? It turns out that the malaria virus has trouble entering a cell shaped like a sickle. Malaria also happens to be a virus that is common in tropical areas. Ultimately, it was theorized that this condition which changes the shape of an individual’s red blood cells endows the host with protection against malaria, and is thus favored because of its benefits. In a tropical place, where the change was advantageous, people with sickle cell anemia were more likely to pass along their genetics to the next generation; whereas people without the sickle cell gene were more likely to catch malaria and die before they could procreate2.
So what happens when you take someone with sickle cell anemia out of the tropics? For instance: take a family from Lagos who moves to Denver. There are not a lot of cases of malaria in Denver, but there is the challenge of high altitude. An unfortunate side effect for people with sickle cell anemia is that, because of the shape of their red blood cells, they cannot carry as much hemoglobin in their blood. These people, because of their genetics, are at a much higher risk for altitude-induced hypoxia3.
Does a person’s genetics influence which dietary plan would work the best for them? Absolutely! A person with phenylketonuria has a genetic condition that prevents them from making the enzyme phenylalanine hydroxylase, making them unable to convert the amino acid phenylalanine to other amino acids, like tyrosine. What do you think would happen if a person with phenylketonuria went down to a steak house and tried to polish off that belly-busting, 72-oz. porter to get a free meal? Beef is high in the amino acid phenylalanine, so if someone with phenylketonuria were to eat a large steak, it could possibly cause them to have a seizure.
Origin of the Blood Type Diet
Dr. d’Adamo tells us that he didn’t actually come up with the blood type diet theory. It was an observation that was made by his father which gave him the inspiration for writing the book. The story goes that his father worked as a physician in some European spas and noticed that some of his patrons were thriving on the vegetarian diet they were given, while others were having struggles like weight gain, digestive issues, and other health concerns. Clearly, this diet wasn’t right for everyone, so he wondered how it could be determined who should eat a vegetarian diet, and who should not. This is how the theory for the blood type diet came to be. Dr. d’Adamo began collecting data, establishing an evolutionary basis for blood type, and researching biochemical compatibilities and incompatibilities involving food and blood type. He compiled this data in his 1996 edition of Eating Right 4 Your Type and has made several revisions and supplementary books to help people choose foods based on their blood type.
It’s a great story! It’s no wonder the diet became so popular, because it results from an exemplary application of the scientific method, which:
- Always begins with an observation about the world. In this case, it was, “Some vegetarians are healthy, and others aren’t.”
- Then a hypothesis follows: “Maybe it is because of their blood type.”
- The next step is to design an experiment, analyze, retest if needed, then draw conclusions.
In coming to his conclusions and validating his theory, Dr. d’Adamo collected historical data and information about chemistry. Our aim here is to address his claims and the claims of others to show what is good about the blood type diet, and what could be improved.
A valuable experiment would evaluate people of various blood types following their recommended diet from Dr. d’Adamo and a control group following a standardized diet. There are a couple of scientific studies that attempted to test his theory in this way. One was the PLOS study that was done in Toronto Canada published in 20144, and there was a Belgian study in 20135. Both independent teams came up with the same conclusion that there is no corollary evidence to support the blood type diet theory.
 Normally, we could stop right there. There was an observation, a hypothesis, an experiment, and conclusions drawn; however, looking deeper into the studies, we can see that the authors didn’t really research the diets very well. To say that their miscategorization of the diets was a gross oversimplification is an understatement. For instance, according to the diet an individual with type AB blood could get away with eating white potatoes, but that doesn’t mean that they can eat potato chips and french fries like this study allowed. This is a problem.
Normally, we could stop right there. There was an observation, a hypothesis, an experiment, and conclusions drawn; however, looking deeper into the studies, we can see that the authors didn’t really research the diets very well. To say that their miscategorization of the diets was a gross oversimplification is an understatement. For instance, according to the diet an individual with type AB blood could get away with eating white potatoes, but that doesn’t mean that they can eat potato chips and french fries like this study allowed. This is a problem.
The other issue, which is rampant among evaluations of all kinds of diets, is that the biomarkers measured are not always indicative of valid health concerns. For instance, someone with high triglycerides is not necessarily going to have a heart attack. It would be best if total cause mortality was the only indicator, because it is easy to manipulate data and statistics with other biomarkers (see the “China Study”6 for a clear example of how to push a vegan agenda by manipulating data). I would love to see an independent study done where the researchers have read and understood Eating Right 4 Your Type, but there does not appear to be one.
The Genealogical History of Blood Type: Blood Type Diet v. The Scientific Consensus
The Blood Type Diet (Simplified):
Let’s start from the beginning. Dr. d’Adamo claims that the oldest blood type (in humans) is O and claims that “O is for Old.” The people with type O blood are supposed to follow a hunter/gatherer type diet and limit grain, legumes, and dairy.
According to d’Adamo, “A is for Agrarian” and it first appeared somewhere in the Middle East between 25,000 and 15,000 BCE. He says that people with type A blood should eat cultivated grain, recommending to them a plant-based diet for optimal health.
Also, according to Eating Right 4 Your Type, “B is for Balance” and claims that type B blood appeared between 15,000 and 10,000 BCE and says that these people can eat meats and dairy, but not wheat.
Finally, according to d’Adamo, the AB type is the newest type, first appearing around 500 BCE. Those with it carry the trait of having low stomach acid. He claims that people with type AB-blood cannot “metabolize [meat] efficiently and the meat you eat tends to get stored as fat.”
The Scientific Consensus:
There are scientists that specialize solely in genealogical evolution. They are not medical doctors, they don’t have patients, and they aren’t writing diet books. Instead, they have devoted their careers to investigating the origin of genes responsible for creating the differences in cell membrane that determine blood type. They look for evolutionary pressures that might explain why certain polymorphisms appeared and why they could be favorable in certain populations. Though there is some debate whether there is evidence that natural selection plays a role in the different blood types at all7.
ABO blood types are not unique to humans, and the alleles that control blood type predate humans by about 2 million years8. This shows that the standard mutation-drift balance model proposed by d’Adamo is clearly out of scope. Chimpanzees have the same ABO blood type variance as humans, even though they have not evolved a system of agriculture, they do not domesticate cattle, and they eat pretty much whatever they can get their hands on. This is quite divergent from d’Adamo’s model, which proposes that type A blood was a genetic adaptation to agrarian life, as chimpanzees have type A blood and have not developed agriculture.
The question remains: Why do we have different blood types? Some claim that there is no evolutionary reason, and others suggest that it is a response to immunity to certain viruses (like in the case of sickle cell anemia and malaria.) Different blood types are determined by different genes. There are genes that express glycosyltransferase proteins which attach carbohydrates to the membranes of red blood cells. If a person has a gene that expresses the glycosyltransferase protein, they will be of a certain blood type, and if they don’t they will belong to another. What is the reason for this genetic adaptation? It is an interesting debate, but there is one thing that we know for sure—the blood type diet’s genealogical model is different from what I consider to be the scientific consensus.
There appears to be a lot of evidence out there that shows all four blood types were around before humans; therefore, the changes of human civilization and lifestyle occurred after the genetic phenotypical presentation. Thus the evolutionary pressures hypothesis of Dr. d’Adamo, according to conventional science, is false. Now, this doesn’t automatically prove that the diet doesn’t work. We must take a lot of these studies with a grain of salt because of the issues with radial carbon dating and the challenges with archeology. A lot of information has been redacted and changed over time.
There is something else to consider along the same line of observation made by Dr. d’Adamo’s own father. The blood type diet theory seems to imply that these hunter-gatherer, agrarian, and Neolithic societies all switched over globally at roughly the same period of time (at least within a few hundred years), but what about aboriginal humans that are living and thriving today? What about the Kalahari, the Pirahã, the Sentinelese, and the Spinifex? Do they all have type O blood? Of course not. Do the members of the tribe who do not have type O blood appear to be any better or worse off than those that do? There isn’t any evidence of this. Shouldn’t we see a person in one of these aboriginal tribes with type A blood that is just having a heck of a time? Sometimes we do. Sometimes we don’t. I would love to see a study done on one of these tribes to see if it is correlated.
Biochemical Support: The Lectin Theory
Eating Right 4 Your Type does not follow the scientific consensus regarding biological evolution, but that doesn’t necessarily make it wrong. What about the chemistry lesson that d’Adamo gives in the book? What are lectins and mitogens? And how does our blood type change the way we react to foods?
Eating Right 4 Your Type begins the molecular biology section with a discussion about the discrepancy in the amount of carbohydrate that we eat (which d’Adamo sets at about 50% of our diet) versus the amount of carbohydrate that comprises the human body (which d’Adamo sets at about 1%). He then talks about the role of carbohydrate in the body (outside of glycolysis) and discusses monosaccharide signaling, and that the A and B blood type groups have differing carbohydrates on the cell membrane, whereas type O does not.
Lectins, or proteins that bind carbohydrates, play a big role in the food selection for each corresponding blood type. Dr. d’Adamo writes about how some lectins are destroyed by soaking or cooking the food, but some are not. He includes a lot of research in the book citing several studies.
These are great bits of research d’Adamo includes. There has been a lot of thought as to the health consequences of eating different compounds and substrates. But what does this have to do with blood type? How does the author arrive at the 16 food categories that are supposed to be “beneficial,” “neutral,” or “avoid” for each blood type? Is there any biochemical basis for these categorical determinations?
What is Blood Type?
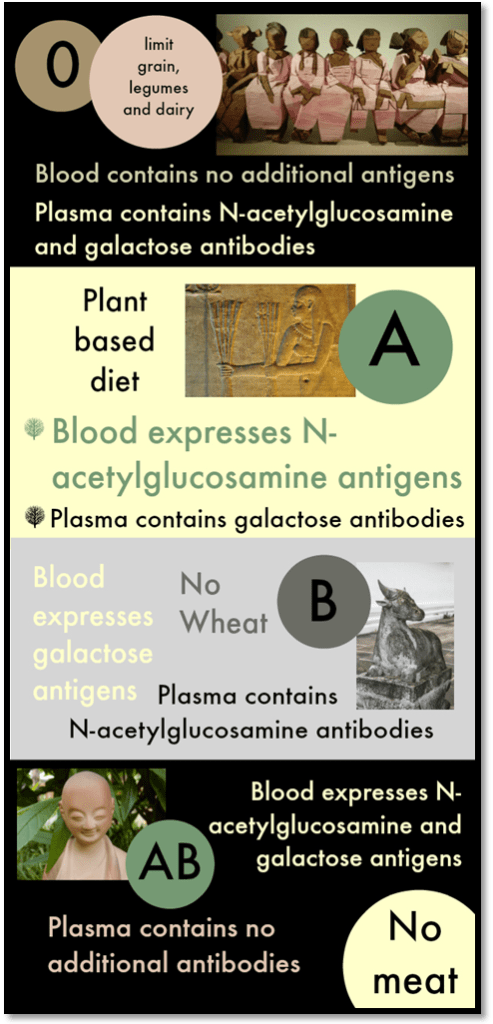
There are 35 identifiable blood types in humans. The vast array of blood types is much more complicated than what is discussed in any of the blood type diet books, and for some reason, the Rhesus antigens are completely ignored in them. In medicine, the ABO system of blood-type categorization is the most commonly used, because it provides the information necessary for blood transfusions. Type O blood is the simplest of the four human blood types because it does not contain Type A or Type B compounds in the cell membrane. Type A blood exists because of a gene that creates an additional transferase enzyme which adds an additional N-acetylglucosamine compound to the cell membrane. Those with type B blood have a different gene that contains a different transferase enzyme which adds galactose instead. In type AB, both genes are expressed and we see both compounds.
Type O phenotype: none
Type A phenotype: N-acetylglucosamine antigens
Type B phenotype: galactose antigens
Type AB phenotype: N-acetylglucosamine and galactose antigens
When we look at the plasma, instead of the red blood cell, we see the opposite.
Type O phenotype: N-acetylglucosamine and galactose antibodies
Type A phenotype: galactose antibodies
Type B phenotype: N-acetylglucosamine antibodies
Type AB phenotype: none
Rhesus Values
There are positive and negative Rhesus values that correspond to each phenotype. These values are not associated with carbohydrate groups attached to the cell membrane, but to proteins. The Rh values are much more complicated, as they contain several protein markers which differentiate them into many more classifications9. Unless you need a blood transfusion, Rhesus value information is more useful than the ABO blood type because of a complication in pregnancy. If the mother and fetus have opposing Rh values, there is a possibility of an incompatibility issue known as Rh sensitization. This condition is rare (especially in the first pregnancy) and is manageable.
Why isn’t Rh important in the blood type diet? According to d’Adamo, Rh is not an important factor in diet, because these proteins are only found in antigen form (in the cell membrane) and not in the antibodies, therefore, they are not present in anything other than red blood cells. He then contradicts himself by discussing “secretor status,” or the presence/absence of antigens in the plasma. If Rh values were to be considered in the book, beyond the 4 blood types (with 2 “secretor” values for each, making 8 total categories) one would have to deal with 35 blood types and their corresponding secretor values.
What is “Secretor Status?”
Everyone has N-acetylglucosamine and galactose somewhere in their circulatory system. The difference between the blood types is that some people have it as an antigen (attached to the cell membrane), while others have it as an antibody, part of their immune system. Both compounds exist somewhere in the system, but Eating Right 4 Your Type places a lot of importance on whether they are present in other bodily fluids like saliva, tears, or mucus. They even have a kit for sale on the website that you can use to determine if you are a “secretor” or “non-secretor.”
The recommended foods change significantly depending on your secretor status. For instance, in Eating Right 4 Your Type, if you have type A blood and you are a “secretor,” you should avoid bananas, but if you are a “non-secretor,” bananas are neutral. If you haven’t paid to take the test, you are told to follow the “secretor” diet.
Scientific Validity of “Secretor Status”
 According to d’Adamo, 80% of the population are “secretors.” The peer-reviewed literature states otherwise. Studies show that 100% of the population expresses antigens into other bodily fluids in type A and type O blood, and 95% in type B and type AB10.
According to d’Adamo, 80% of the population are “secretors.” The peer-reviewed literature states otherwise. Studies show that 100% of the population expresses antigens into other bodily fluids in type A and type O blood, and 95% in type B and type AB10.
How could these values be so disparate? A modern technique known as the absorption inhibition method was developed in the field of forensics that detects antigens more reliably than the saliva swab test kit sold on the dadamo.com website11. As the reliability of testing increases, it could be reasoned that detection of antigens in type B and type AB would increase to 100% with advancing technology. Just because the antigens can’t be detected does not necessarily mean that they are not present.
Another point of discussion is the type O antigen secretion. If you look at the blood type chart above, you will see that type O blood is determined by the absence of N-acetylglucosamine and galactose antigens. How is it possible to be a “secretor” when there is nothing to secrete? In fact, there are compounds in the antigens that are excreted, but they are not related to the nonexistent carbohydrates. This is useful for law enforcement agencies that are trying to convict a criminal (or a legal defense team trying to exonerate an innocent person), but how is this helpful in the blood type diet?
This is a little confusing because the blood type diet focuses on lectins in foods and their ability to bind to carbohydrates. The carbohydrates of interest are N-acetylglucosamine and galactose because that is what differentiates blood group, but O antigens do not have either of these carbohydrates. If the only compounds of note are not being secreted either way, why does it matter? Why would a “non-secretor” be able to eat quail and turtle, but a “secretor” cannot? The point is moot because there is no such thing as a type O “non-secretor,” but I would be interested to know the rationale for this dietary recommendation.
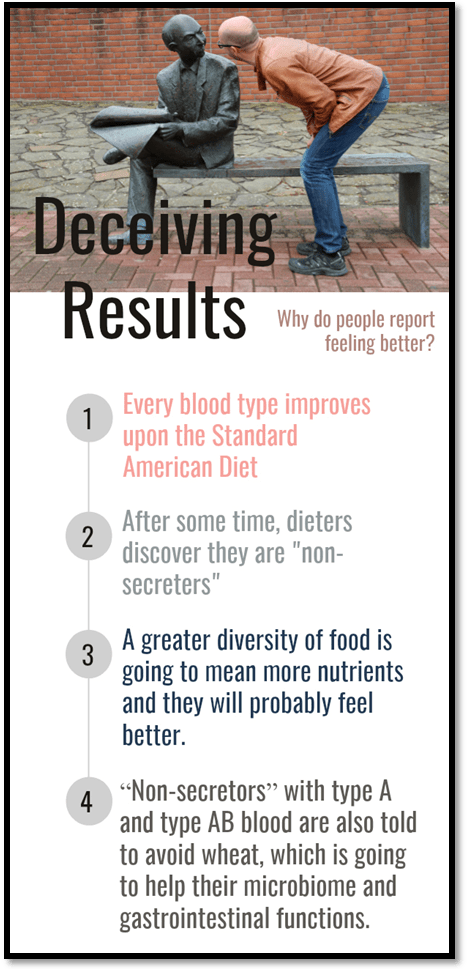
If you browse the blood type message boards and read independent blogs, you will find people who have purchased a test kit from the dadamo.com website and claim to be type A or type O “non-secretors” despite the evidence to the contrary that these designations are impossible. Some have even made dietary changes after learning their “secretor status” and have demonstrated positive changes in their health. We know that if we used the absorption inhibition method, we would find the corresponding antigens that went undetected. So, why are they experiencing benefits? When a person first begins the diet, they are told to assume that they are a “secretor.” Then, when they do the saliva test, and it tells them that they are a “non-secretor,” then they can add more foods into their diet. A greater diversity of food is going to mean more nutrients and they will probably feel better. “Non-secretors” with type A and type AB blood are also told to avoid wheat, which is going to help their microbiome and gastrointestinal functions.
The Lectin Theory
The biochemical premise of Eating Right 4 Your Type is as follows:
-
- There are lectins in everything we eat.
- Lectins bind carbohydrates.
- Carbohydrates are in some of the components in our blood.
- These carbohydrates differ by blood type.
- Different lectins bind to different types of carbohydrates.
- Therefore, we should base what we eat on our blood type.
Ricin
Castor oil seeds contain a lectin called ricin. If you watched the television series, Breaking Bad, you might remember the scene where they extract ricin concentrate to kill a bad guy. It was a good strategy, because even a small amount of ricin the size of a grain of sand is lethal to humans. The LD50 (median lethal dose) of ricin is only 22 milligrams12. Why is it such a lethal compound? Ricin binds the carbohydrate, N-acetylgalactosamine. (You might remember this compound from the discussion of blood type above.) Ricin is so efficient at binding these carbohydrates that it can bind to cell surfaces in the order of 106 to 108 times greater13. This lectin is also unusual because it forms such a strong bond that it acts almost as an rRNA N-glycosylase enzyme, meaning that it can potentially break the sugars off from their proteins14. In this process, the adenine residue picks up a hydrogen atom to stabilize the compound, which is what inevitably causes the irreversible damage to the RNA15. In other words, the ricin lectin attaches to a specific sugar found in the cell, snaps it off, and it forms a compound that prevents you from synthesizing proteins, ultimately killing you.
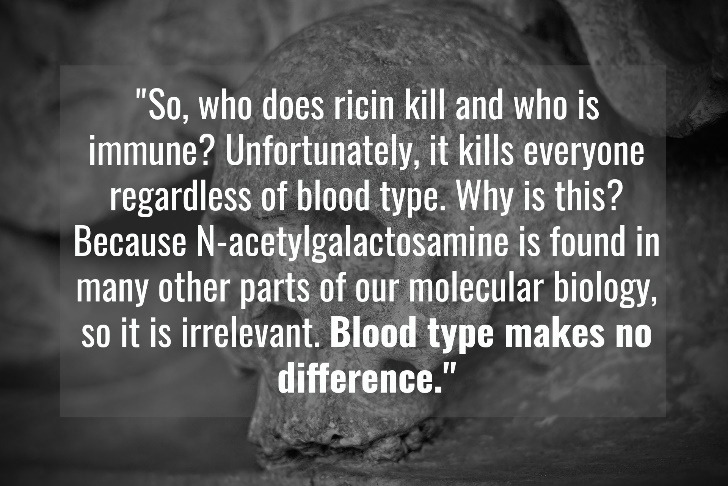
Who is safe from ricin poisoning? People with type A, type B, or type O blood? Ricin binds to N-acetylgalactosamine, which is found in the antigens of type A and type B blood, but it is also found in the antibodies of people with type B and type O blood. So, who does it kill and who is immune? Unfortunately, it kills everyone regardless of blood type. Why is this? Because N-acetylgalactosamine is found in many other parts of our molecular biology, so it is irrelevant. Blood type makes no difference.
Biochemical Sensitivity to Foods Based on Antigens and Antibodies
The next logical step is to try and find a biochemical connection between compounds in foods and N-acetylglucosamine/galactose antigens or their antibodies. Dr. d’Adamo claims that there are some connections there and writes about various compounds in Eating Right 4 Your Type.
Wheat Germ Agglutinin
Wheat germ agglutinin (WGA) is a lectin that d’Adamo describes in Eating Right 4 Your Type. He cites some human studies and concludes that type A “agrarian” individuals are fine with wheat, as well as those with type AB blood (so long as they are “secretors”), but non-secreting type O’s and type B’s should avoid eating wheat. According to d’Adamo, N-acetylglucosamine antigens protect a person from this WGA.
WGA is compound that binds to N-acetylglucosamine, which is a component of the antigen in type A blood cells, but a component of the antibodies in type O and type B blood cells. N-acetyl-D-glucosamine is also found in the chitin of the exoskeleton of insects, and it is thought that wheat evolved this lectin as a protection mechanism.
Theoretically (and only theoretically, because it would be a crime to actually do it), if we injected WGA into a person’s bloodstream, we would find WGA binding to the membranes of people with type A blood, and the antigens of those with type O and type B blood. We would also find WGA binding to any matrix or membrane containing N-acetylglucosamine.
The two most common areas for binding are cartilage and corneal tissues. Why are these lectins binding to these tissues and not to the blood cells or antigens? They can do the latter, but it is temporary. This is because of entropy, or Newton’s Second Law of Thermal Dynamics. As d’Adamo correctly states in Eating Right 4 Your Type, when WGA binds to N-acetylglucosamine, it is not a covalent bond. At the pH of blood, it doesn’t take much force for the carbohydrate to detach16. WGA will be carried by either the blood cells or the plasma (depending on the blood type) until it reaches a larger concentration of N-acetylglucosamine perhaps in the cartilage or the eyes. How do we know that this is correct? WGA can be labeled using a fluorescence technique, as can the substrates to which it binds17. It’s one thing to have a theory about how something works, but it is another to label the compounds and watch what happens to them both in vitro and in vivo so that the transport and binding mechanisms can be confirmed.
No matter what your blood type, WGA will bind to tissues with stronger concentrations of N-acetylglucosamine. That is what is predicted by physics, confirmed in fluorescence observations, and what we consistently see in peer-reviewed literature. There are studies showing the binding of WGA to the extracellular matrix of cartilage in vivo18, as well as studies showing the binding of WGA to the central cornea19. It is important to mention that the studies that show WGA concentrations in vivo were done in rats, not humans, because it would be unethical to inject humans with WGA. Rats do not have the ABO blood type that humans do, but they have A, O, and another type called M20. They possess N-acetyl-D-glucosamine antigens and antibodies. If we performed this experiment in humans (again, which would be a crime), we would expect to see the same result. This is one of the reasons why people who don’t abstain from wheat sometimes complain of sore joints and inflamed eyes—especially if they have a thin mucosal membrane in their intestines, bacteria whose biofilms have penetrated the membrane, or eat other compounds that create a lot of osmosis in the small intestine which leads to the opening of the tight junctions.
WGA does not appear to be beneficial for any human regardless of blood type or secretion status. There are no clinical examples of people with N-acetylglucosamine antigens that can negate the damage of WGA. People who do not show immediate damage from eating wheat tend to have an optimized microbiome, a fast MMC, no signs of water retention, and a thick mucosal membrane. None of these factors have anything to do with blood type.
Eating Right 4 Your Type doesn’t put wheat into the “beneficial” category for any of the blood types, but if you are following a blood type diet, I would discourage you from eating it even if you are a type A “secretor.” At least try it for 30 days and see how you feel.
Banana Agglutinin (BanLec)
Bananas are brought up quite a bit in Eating Right 4 Your Type. They are a recommended food for type B “secretors” and for all people with type O blood. The rationale behind this is related to agglutinin expressed by the BanLec gene. Dr. d’Adamo proposes that the presence of galactose antibodies is a winning combination with agglutinin and he believes that it will keep people from getting sick. People with type AB blood should avoid bananas and type A “secretors” should avoid them too, because the agglutinin will slow down their metabolism.
Dr. d’Adamo proposes that agglutinin “flocculates serum or precipitates serum proteins.” What does that mean exactly? It means that there is some sort of a protein that is found in type AB and type A “secretors” that reacts to this lectin. But wait! I thought lectins bound carbohydrates! According to Dr. d’Adamo, the BanLec lectin somehow pulls the protein out of position and collects into small molecular clumps in the plasma. The result is that metabolism slows.
I tried my best to find any sort of research to validate this, or invalidate it. The issue is that the banana agglutinin is in the jacalin family of lectins and it binds to mannose21. This makes it hard to determine which substrate is supposedly being pulled out from the serum, what sort of colloid is forming, and what effect this would have on the mitochondria. Logically, there must be some sort of glycoprotein containing mannose used somewhere in a glycosylation process, so I browsed through several gene catalogs and looked for a substrate with two shared elements:
- It must be a serum antigen glycoprotein that contains mannose.
- It must be unique to people who only have type A antigens.
Mannose contains symmetry in the carbon ring because the hydroxyl groups are displaced from the ring to not interact with the central oxygen atom within the ring. This is quite different from N-acetylglucosamine, which contains an amine group and does not contain the same symmetry. This is important to visualize, because in organic chemistry, we think of antigens and antibodies like keys, and lectins like locks. The key must fit the lock. BanLec22 (or banana agglutinin) contains a series of amino acids that under normal conditions contain 4 beta sheets with internal folds that match the symmetry of mannose. N-Acetylglucosamine is not the correct key to this lock, so we can forget the compounds that bind with N-acetylglucosamine as d’Adamo suggests.
The absence of evidence is not the evidence of absence however, so there could be some mystery compound out there that has yet to be discovered which makes d’Adamo’s theories somewhat valid. However, there are some other noteworthy contradictions that seem to invalidate or at least demonstrate some convolution in d’Adamo’s understanding of lectins—or maybe I am the one who is confused. I looked up some of Dr. d’Adamo’s medical textbooks to get a clearer understanding of why he thinks this way. Unfortunately, when I looked up his reference for this information, he ends up citing himself as the source. That’s not very helpful!
I then had to interlibrary loan other texts, and it was all circular. He’s got this model in his head, but he doesn’t have any support other than what he has written on the biochemical process his theory relies on. If this science holds true, why hasn’t it been observed or documented? And if it has been observed or documented, why doesn’t d’Adamo cite the primary research instead of circling back to his other writings?
The BanLec protein was the first jacalin protein to be discovered, but there have been several others. Jerusalem artichokes contain a lectin similar to BanLec, and its discovery has some implication on the widespread use of mannose binding lectins and their genetic advantage in the plant kingdom. In Eating Right 4 Your Type, bananas are to be avoided for people with type A blood, but Jerusalem artichokes are a recommended food because it “contains a component which positively influences known disease susceptibility.” Why is this? How are the carbohydrate-binding properties of BanLec different from 1-3Man, the lectin in artichoke?
We find a similar contradiction in the blood type diet for people with type O blood when we look at barley. People with type O blood are to avoid barley because it is a “metabolic inhibitor.” Barley contains a lectin called HL#2, which is another mannose-specific binding protein in the jacalin group23. Research points to the same conclusion for this lectin as with the BanLec. Although, it has a slightly different binding site, it has the same mannose-binding properties as HL#224. So again, we must ask why is it recommended for type O people to consume bananas, but barley is to be avoided? They contain functionally similar lectins. Why is it recommended for one, but avoided for the other?
In some of Dr. d’Adamo’s other writings, he demonstrates an understanding of jacalin lectins and he addresses jackfruit, Jerusalem artichokes, and bananas, but there are a lot of other plants that contain the same class of lectins. When you look at the dietary recommendations, it is all jumbled and it is not very specific about plants and lectins. Also, mistakes are made in the categorization of blood group recommendations.
I don’t know exactly where the breakdown took place. Was it a lack of research? Are there other lectin groups that take precedence over others? The point is somewhat moot because the chemistry is unsupported in any case. It’s one thing for a blogger on the internet to put links to other pages in the same blog, but in a scholarly article, you cannot cite yourself unless you conducted the primary research. And Dr. d’Adamo has not to my knowledge done any primary research in molecular biology.
 My issues with bananas and plantains tends to derive from their resistant starch content. People who consume a low-carbohydrate diet tend to incorporate them into their diets because it doesn’t affect blood sugar values, yet it acts as a prebiotic in the gut, so some people find that it is helpful, but others (like people who suffer from Klebsiella overgrowth) suffer from a lot of issue from banana and plantain starch. In both cases, the health effects are not associated with the proteins in the bananas (like in the case with BanLec) but with the carbohydrates that supply energy to microbial life in the digestive system. There is a lot of science supporting bacterial interactions with starches, and many papers have been written on the subject that are not hard to find. Therefore, it is much more likely that the microbiome should have a greater impact on the dietary recommendation of bananas and plantains than a person’s blood group.
My issues with bananas and plantains tends to derive from their resistant starch content. People who consume a low-carbohydrate diet tend to incorporate them into their diets because it doesn’t affect blood sugar values, yet it acts as a prebiotic in the gut, so some people find that it is helpful, but others (like people who suffer from Klebsiella overgrowth) suffer from a lot of issue from banana and plantain starch. In both cases, the health effects are not associated with the proteins in the bananas (like in the case with BanLec) but with the carbohydrates that supply energy to microbial life in the digestive system. There is a lot of science supporting bacterial interactions with starches, and many papers have been written on the subject that are not hard to find. Therefore, it is much more likely that the microbiome should have a greater impact on the dietary recommendation of bananas and plantains than a person’s blood group.
Legumes
There is a lot of discussion about the interaction between legume lectins and the microbiome in Eating Right 4 Your Type. Dr. d’Adamo writes about the interaction between various compounds from legumes and provides some very good research to go along with it. I found it to be very accurate and noted his reference to a lot of studies that we often cite here on Fix Your Gut.
Legumes seemed to evolve their lectins because of an evolutionary pressure to increase their supply of nitrogen. Any farmer worth their pitchfork will tell you that planting beans is good for the soil because they are “nitrogen fixers.” Nitrogen is the most common element in the Earth’s atmosphere, but it doesn’t bind with soil very well in its gaseous form. If the presence of legume plants increases nitrogen levels in the soil, they must have a way to convert nitrogen in the air to a compound that can be used in the soil, right? It turns out that the legume plants themselves cannot do this, but several types of bacteria can. It has been proposed that the genes responsible for making the lectins found in legumes evolved to serve the genetic function of attracting and binding bacteria so that nitrogen would deposit by the plant’s roots. Crop rotation has been used for countless generations, and we can witness the benefits of legume genetics applied in agriculture dating back hundreds of years.
Legumes are great for soil, but they are not always great for the gut. The same bacteria-attracting properties that legumes have in agriculture also apply in the human digestive system. Dr. d’Adamo addresses several of these concerns in Eating Right 4 Your Type and makes references to many quality studies, but it is not clear what this has to do with blood type. It makes sense that these lectins can cause problems, and I agree with the studies he discusses, but I do not see a clear tie to blood group.
Phytohemagglutinin lectin in kidney beans can cause a lot of gastrointestinal distress. Eating them raw can even be lethal, but soaking and cooking them brings them down to “safe levels.” (I put “safe levels” in quotes, because eating kidney beans is still not a good idea for everyone.) As with my ricin example in my “Lectin Theory” section of this article, phytohemagglutinin from raw kidney beans can kill anyone regardless of their blood type. No one is immune.
So, why can some people eat kidney beans and not have any problems, but others get symptoms like gassiness, inflammation of the intestines, constipation, and/or autoimmune issues from them? The research tells us that this has a lot to do with the microbiome, or the bacterial component of the human gastrointestinal tract. People who have greater numbers of bifidobacteria tend to have a stronger mucosal membrane because bifidobacteria are great at turning starch into short-chain fatty acids like acetic and butyric acids, which are integral in forming the mucosal membrane25. The mucosal barrier protects the epithelial cells lining the intestines from the irritating lectins in the beans.
Dr. d’Adamo claims that your blood type influences the bacterial composition of the human microbiome. Therefore, someone with type B blood must have higher quantities of bifidobacteria and thus more resistant to the lectins in kidney beans. It makes sense, but only if there is a link made to the microbiome.
Blood Type and the Microbiome
Dr. d’Adamo claims that your blood type has an influence over the types of bacteria in your gut., but there wasn’t much in the scientific literature to confirm this theory until 2012. A study performed by members of the Finnish Red Cross and two representatives from a DuPont-owned company called Daniso, which manufactures foods and dietary supplements, sought to test this theory26.
Could ABO blood type influence the microbiome? The study collected 79 volunteers who were “non-secretors” and collected blood and fecal samples. (If you have read the section of this article on secretor status, you probably have already identified a problem with this study.) The participants were categorized by blood type and their fecal matter was run through polymerase chain reaction with denaturing gradient gel electrophoresis (PCR-DGGE) to determine the microbial content against a library of bifidobacteria: B. longum, B. adolescentis, B. bifidum, and B. catenulaturn gr.. They also claimed to have tested Lactobacillus, but do not show any difference in microbial content for the ABO blood groups. In the conclusion paragraph, they claim to have recently tested “secretors” and “non-secretors,” but the data is missing.
What does the data actually tell us about the connection between blood type and microbiome? I looked at the raw data, the graphs, and the statistical graphs and easily made the determination that there are no statistical trends. The plots are completely random. How did they conclude that these bacteria were correlative to the ABO blood groups? Also, mathematically, if your mean blood group variable differentials are less than the standard deviation, how can you claim that it is correlated? The article goes into a lot of explanation about the accuracy and validity of PCR-DGGE, but does not contain a single bit of statistical information. There was none whatsoever.
 So, how did they come to this conclusion? Did they test it against the base Finnish population? What were the controls? There are so many issues with this study, I can hardly imagine why the folks at BMC Microbiology published it. Did they even read it? According to their policy, “BMC Microbiology operates a single-blind peer-review system, where the reviewers are aware of the names and affiliations of the authors, but the reviewer reports provided to authors are anonymous.”27 I have reached out to the authors of the study and to the publisher and asked them how they can show correlation when their plots look like a Jackson Pollock painting. They did not respond.
So, how did they come to this conclusion? Did they test it against the base Finnish population? What were the controls? There are so many issues with this study, I can hardly imagine why the folks at BMC Microbiology published it. Did they even read it? According to their policy, “BMC Microbiology operates a single-blind peer-review system, where the reviewers are aware of the names and affiliations of the authors, but the reviewer reports provided to authors are anonymous.”27 I have reached out to the authors of the study and to the publisher and asked them how they can show correlation when their plots look like a Jackson Pollock painting. They did not respond.
In 2016, similar research was performed in the United Kingdom. The participants included 1,503 twins (I know, it’s an odd number—don’t ask me to explain) from the TwinsUK registry28. They sorted the participants into their ABO blood groups and tested using the same PCR-DGGE method as with the Finnish study. They carry out a broader, and frankly more accurate (e.g., showing why they used bifidobacteria), analysis looking at the ruminococcaceae and lachnospiraceae families, rather than species-specific strains. Like the other study, they tested based on secretor status (which is a little troubling), but they came to the exact opposite conclusion. They say that neither ABO blood type nor secretor status has any correlation with the microbiome.
Why does the Finnish study come to a positive conclusion, while the UK study comes to a negative one, regarding ABO blood type correlation with the microbiome? The scatter plots look similar, but the UK study has more data points. How could this be? The UK study had a predefined Q-value, and the authors specifically noted how they used their statistical equations to draw a conclusion. The Finnish study did not. If I could get the raw data from the Finnish study, I could run it through the formulas listed in the UK study and see if there was a correlation, but unfortunately, I do not have this information.
Which study is more likely to address the global model? Based on what I see, the UK study is more likely to be valid because they used families rather than species (which lends itself much better to PCR testing), and they are transparent with their mathematics. If I find otherwise, I will amend this article and post the reply from the authors with the newly provided data.
It is concerning to me that in both studies, they are still referring to obsolete terminology that created a system of knowledge which arose from poor detection techniques. Detection methods have come a long way since the 1950s when the “secretor status” philosophy emerged. Before starting a study, there should be a long, careful research phase to see what has already been done in the area of study, and how the proposed study fits into the current published body of literature. Through this process, this discrepancy should have been uncovered.
H. Pylori
H. pylori is a species of bacteria that we write a lot about on Fix Your Gut. It is a part of the natural gut flora, but there are several genomic factors that can lead to pathological overgrowth of H. pylori, causing gastrointestinal disease including ulcers, acid reflux, and heartburn. Some people seem to be highly susceptible to H. pylori infections, while others are asymptomatic. We have theorized about genetic factors that could allow for a greater risk of H. pylori overgrowth and have explored the expression of different T helper cells as a predicting factor, but there is a lot of theory and no observable science. Could ABO blood group be that missing link?
There have been some studies written about ABO blood group and its effect on H. pylori infections in symptomatic patients29. It is interesting material. It shows that people with type AB blood are much less likely to have H. pylori infections than someone with type O blood. Supporting literature shows that people with type O blood have a much higher risk of stomach ulcers30. Another interesting component to the study is that 92% of people with positive Rh values were deemed to have H. pylori infections.
The problem with H. pylori infections is somewhat similar to that of strep throat. If you were to walk into any elementary school and swab four random kids (which would be a crime by the way, so please do not do this), you would find that three of them came back positive for Streptococcus even though they had no fever or sore throat. Doctor’s offices perform these tests and often prescribe antibiotics to people who have viral infections. The diagnostic test is problematic because Streptococcus is a part of the natural human flora. Unfortunately, so is H. pylori, but H. pylori is much more difficult to detect. Everyone has H. pylori as a part of their natural flora. In fact, I challenge anyone reading this to try and find a public water supply that does not have H. pylori bacteria swimming around in it.
There are many patients who are clearly symptomatic of H. pylori overgrowth and upper gut infections, but the detection methods are not always able to detect it. Sometimes, the symptoms go on for years before they are finally diagnosed and treated. The ABO blood group studies on H. pylori are interesting to me, but I am not confident enough in the detection methods to trust the findings. Perhaps the antibodies in type O blood mask the antibodies to H. pylori. Perhaps there is something else going on. We could theorize all day, but without data, the speculation has little value. This should only encourage us to research further.
The Salt-Stressed Rice Paradigm
There is something that needs to be considered when making claims about food. Not every piece of produce is completely uniform in nutritional content. For instance, if you buy strawberries, sometimes they’re sweet and sometimes they taste sour. Why is this? Some of it is genetics. Farmers tend to cultivate produce that is more palatable, because it sells. Over generations of breeding, we tend to find less bitter vegetables for instance, and sweeter-tasting fruit that is aromatically pleasing. Generally, over time you get higher yields, smaller and fewer seeds, and larger edible portions. Many of these plants would not have existed naturally if it weren’t for this process. When you see a citrus tree that is being held up by stakes and supports, it is obvious that that cultivar could not have survived on its own. Its limbs would have snapped off in the wild, and it would die. These adaptations were not genetically advantageous to the plants, but they were catered for our consumption (presumably).
Many of the compounds that we find in produce (desired or undesired) are a result of environmental stimulation. In the wild, how does that (or how did that) organism deal with life-threatening factors like insects, fungi, drought, and environmental toxins? Blueberries, for instance, when under stress from insects synthesize more anthocyanins. Why? There is a high metabolic cost to producing them. This process is evolutionary advantageous to the species because anthocyanins are antibacterial and antifungal, preventing damage to the fruit31. Looking at other stress factors to the blueberry plant, we see that light, drought, and cold temperatures lead to a higher concentration of anthocyanins as a stress response adaptation.32
Anthocyanins found in blueberries are powerful antioxidants that have been observed to promote health and prevent disease33. Eating Right 4 Your Type has blueberries as a recommended food choice for every group, but how much anthocyanin is in the blueberries that we eat? A lot of it has to do with the environmental conditions that the plant was under before harvesting. The more stress, the more anthocyanin. Well, how much stress are our blueberry plants under in agriculture? What with pesticides, irrigation, antifungals, and other modern agricultural techniques? It is probably fair to say they do not produce as much anthocyanin as their wild counterparts. Why? Because anthocyanins are a biologically expensive compound to synthesize, meaning that the plant must expend a lot of resources to make it. In nature, it is biologically advantageous for an organism to conserve energy rather than to expend it, so there must be a significant enough external stimulus for the plant to invest in the production of anthocyanin. In modern agriculture, plants are protected by human technological innovation, so energy output is focused on yields and not necessarily on beneficial compounds.
What does this have to do with lectins? We can apply the same reasoning to lectins as we can to anthocyanins in blueberries. Lectins are not always expressed uniformly in the plant and animal kingdoms. They are produced as a result of environmental stimulation. We call the area of study surrounding this somewhat counterintuitive phenomenon epigenetics.
Most of the water on our planet has a salinity level of 35 ppt (parts per thousand). Much of the agriculture that sustains human life on this planet cannot survive with a salt content above that threshold. This has an impact on agriculture because farmers must plant crops and water animals with water that is reduced in salt. When a plant is irrigated with water that contains too much salt, it becomes stressed.
Rice responds to biological stress by producing a lectin called orysata, which is a lectin that binds the sugar mannose34. Before a new discovery, it was theorized that orysata evolved to protect the rice plant from insects35, but modern research shows that it is an adaptation to salt36. Either way, the environmental conditions have a direct impact on the lectins produced in rice.
In Eating Right 4 Your Type, it is recommended that people with type AB blood eat rice, because as Dr. d’Adamo proposes it contains an agglutinin (or lectin) that helps to prevent disease. Which disease? It doesn’t say, but the important question that we must ask is: Are these orysata lectins in the rice that people are eating? Not unless they were stressed from salt water, and most of the produce that we eat was grown in ideal conditions where the amount of salt in the water was low.
Location and Concentration of Lectin
 When we look at the function of a lectin protein, it helps to understand the full genomics of the protein. In other words, we need to be able to answer the following questions:
When we look at the function of a lectin protein, it helps to understand the full genomics of the protein. In other words, we need to be able to answer the following questions:
- What gene expresses the protein?
- What are the activators and restrictors that influence its expression?
- What does the protein do (chemically)?
- What was the evolutionary pressure that led to this genetic adaptation
As we learned from the example of salt-stressed rice, not every gene is expressed in an organism all of the time. There are environmental factors that come into play. Many genes are location specific, where a gene within an organism expresses itself to a great degree in one area, and not at all in another. If this weren’t the case, we would have toenails growing out of our eyelids, and in that location, a toenail would cause more problems than it would solve.
Where are lectins found in foods? If you have a lectin expressed in a root vegetable with the function of binding a carbohydrate found in the exoskeleton of an insect, where would you expect that lectin to be present? In the root system, or in the leaves? Insects chew on the leaves of the plant, so we should expect to see the lectin produced there. Unless the root system is under the same pressure, you shouldn’t see high concentrations of lectin in the roots.
Eating Right 4 Your Type does not address the matter of lectin location. In one instance, Dr. d’Adamo cites some research about a lectin he found in a sweet potato plant, makes some tangential connection to human biology and blood group, and places that food in a category. In several cases, the lectins discussed are not even found in the location of the part of the plant that we eat.
Glycomics
Dr. d’Adamo has written another volume of books called Fundamentals of Generative Medicine. One of the biggest topics that he addresses therein is the concept of glycosylation, which is a chemical process that attaches a carbohydrate to another compound. This is an important concept to understand, because the differences in blood type are categorized by the different (or lack of) carbohydrate antigens found in the outer membranes of the red blood cells. He does a good job of categorizing the different glycan groups by their attached compounds, and goes on to classify and describe lectin groups.
Dr. d’Adamo then extrapolates this information and applies it to the human gastrointestinal system. His claim is that we digest food differently based on variations in the expression of glycosyltransferase proteins (the proteins that attach to carbohydrates). He says that the way we secrete these compounds into our fluids affects things like gastrointestinal pH and digestive enzymes. This is where the most obvious mistakes are made in the book, and its claims are a clear defiance of the science that makes up the consensus for basic digestion and metabolism.
If your body can’t digest it, does it turn to fat?
The claim that Dr. d’Adamo makes regarding glycomics is that the interaction between the lectin in the foods we eat and the glycosylation of red blood cells (and how they secrete in the human GI) affects the way we digest foods. He writes that these compounds affect the way enzymes unfold, which in turn has an impact on how they unfold. His conclusion is that a person’s digestive enzymes fold in a different way depending on a person’s blood type. Further, he claims that if a person eats food that they can’t digest (because of their blood type) it turns to fat.
The concept that undigested food turns into body fat is completely wrong. It defies the laws of physics. In human metabolism, fat is an energy substrate, and body fat is stored energy. There is something called the conservation of energy. The total energy of an isolated system must remain constant in that energy cannot be created nor destroyed. Metabolic energy in the body comes from the macronutrients fat, carbohydrate, and to a lesser degree, protein. We have systems in the body that are designed to metabolize these compounds to use for ATP so that our muscles can contract, neurons can fire, compounds can be synthesized, and so on. We can also store this energy as body fat, glycogen, and even our lean body mass can be cannibalized for energy.
Let’s use a basic example of what Dr. d’Adamo is claiming, and why it doesn’t make sense. Let’s say you eat chicken and you have type B blood. According to d’Adamo, you cannot digest chicken properly because of your individual glycosylation, so it will be stored as fat. (Never mind that the first civilization to cultivate chickens was China and someone of Chinese descent is 19% more likely to have type B blood.) If this were true, how would the energy be extracted from the chicken in order to be stored as body fat? Clearly, this is not a balanced energy system. There is energy in favor of body fat with no source. If the chicken foodstuffs are not digested, then they are passed instead of metabolized. We can see an example of this with dietary cellulose. Humans lack the beta acetal linkages to digest cellulose and so it is passed as stool. It isn’t digested. It isn’t metabolized. It isn’t used for energy. It simply moves through the digestive tract and excreted.
When we look at gut health, there are many foodstuffs that humans do not digest efficiently. Part of the problem in the Standard American Diet (SAD) is that people consume a lot of proteins, fats, and carbohydrates that are resistant to human digestive enzymes so they make it all the way to the small intestine. There are bacteria that live in the small intestine that digest and metabolize these compounds much more efficiently than humans. When they are kept well fed, they multiply in number, which can lead to a disease called SIBO (small intestinal bacterial overgrowth). SIBO is real. SIBO has been documented and studied in biomedical literature. We should focus our diets on what we know instead of what we don’t know, and avoiding compounds that lead to SIBO is much more important than unproven, undocumented theories of any sort.
Does Blood Type Affect Your Digestion?
Glycosylation is ubiquitous in the human body. It is happening in every cell, every second of every day. The process that is described by Dr. d’Adamo is lectins interrupting glycosylation, wherein lectin grabs a carbohydrate before it can be used in glycosylation, thus stopping the process. Digestive enzymes are proteins made of a series of amino acids encoded from RNA. Specific lectins can attract sugars like ribose away from the RNA (the ‘R’ stands for ribo-) so that the reaction shuts down. This absolutely happens, with ribose sugar and many other sugars. It is documented, and the mechanics have been observed and identified. Extrapolating this information and applying it to blood group has not gone under the same degree of study and scrutiny.
Dr. d’Adamo looked at the medical literature and found some examples of gastrointestinal disease linked to blood group. People with type A blood have a higher risk of developing gastrointestinal cancers37, and people with type O blood have a higher risk of peptic ulcers38. Though the authors of papers written about these increased disease risks claim not to know why this relationship exists, Dr. d’Adamo believes that his diet will lower the risk. Looking at his diet recommendations for people with type A blood, it very well could.
ABO Blood Group and Stomach Acid
Dr. d’Adamo believes that people with type O blood have too much stomach acid, and that is why they are prone to ulceration. He cites a study from the 1950s to back up his claim39. Biomedical science has come a long way since then.
From a scientific standpoint, there are several problems with the study. It compares people with type O and type A blood groups and claims that it’s not type O that has excessive stomach acid, but type A that has low stomach acid. Neither claim is verified from the study because Sievers doesn’t measure stomach acid at all—he measures plasma pepsinogen, which at a low enough pH will unfold into the digestive enzyme pepsin. Acidity is not measured by enzymes—it is measured by the potential of hydrogen (pH).
Further on in his writing, d’Adamo cites another paper from the same author. The study is similar to the first in that stomach acid is never actually tested. The second paper is even less valid in this argument because it was not performed on healthy individuals, but on people with gastrointestinal disorders. In either case, Dr. d’Adamo misrepresents this information and suggests that there was less hydrochloric acid in the stomachs of the study’s subjects. This is not logical because hydrochloric acid levels in their stomachs were never tested at all.
Dr. d’Adamo goes on to describe a process in which epidermal growth factor (EGF) is responsible for the repair of the gastric lining, but states that EGF “has a high affinity for the type A antigen.” For this to be true, something about the N-acetylglucosamine carbohydrate would have to attract the EGF protein through electromagnetic force toward the EGF binding site of the cell membrane. Looking at the chain of 53 amino acids40, we can predict the possibility of chemical attraction. When we compare it with the cell surface receptor (the “lock” to the EGF “key”), we do not see enough similarity to this ligand group41.
Looking at the Gibbs free energy system, would the presence of N-acetylglucosamine influence the binding of EGF to its receptor site? Could a butterfly flap its wings and create a typhoon on the other side of the world? Chaos theory says yes, but these mathematicians aren’t necessarily recommending the mass extermination of butterflies. In other words, just because it can happen doesn’t mean that it is happening—and there is more evidence than not that it isn’t.
Stomach Acid Does Not Cause Ulcers
If there is one thing that you remember from this article, it should be this: If your doctor ever puts you on a proton pump inhibitor (PPI), you should immediately fire your doctor. PPIs should be on the DEA Schedule I drug list because they can only do harm and they have no value in medicine. That’s because stomach acid does not cause ulcers. Microbes cause ulcers. Stomach acid keeps microbes like H. pylori in check. When H. pylori (which are a part of the natural flora) become opportunistic enough to build up biofilms to protect them from gastric fluid, they excrete urase to shut down the proton pumps that are responsible for creating hydrochloric acid in the gut42. Taking a PPI will only make matters worse. People who have been duped into taking them are in an unfortunate situation, because:
- PPIs do not cure their GI problems
- It is hard to get off of a PPI
 Just to be clear, Dr. d’Adamo does not recommend PPIs in any way. I just wanted to include that information because it is an example of a major misconception in current medical science. Dr. d’Adamo claims that people with type O blood have excess stomach acid and therefore they have more stomach ulcers. This defies the mechanism we understand about stomach acid and opportunistic overgrowth. So, I completely disagree with his recommendation to avoid acidic foods.
Just to be clear, Dr. d’Adamo does not recommend PPIs in any way. I just wanted to include that information because it is an example of a major misconception in current medical science. Dr. d’Adamo claims that people with type O blood have excess stomach acid and therefore they have more stomach ulcers. This defies the mechanism we understand about stomach acid and opportunistic overgrowth. So, I completely disagree with his recommendation to avoid acidic foods.
However, if you look at his type O diet recommendations, you will also find that there are no significant sources of sucrose (table sugar), which heavily influences the ratio of H. pylori to Lactobacillus strains in the gut. Through this dietary intervention, people who are on the diet will be less likely to get stomach ulcers, but if they do, they should seek a remedy that chelates the biofilm and kills the microorganisms. This could be done through antibiotics, or it could be done naturally by lowering the gastric pH to regulate the population. The natural approach has its advantages of course, but in clinical practice compliance is a huge issue, and unfortunately antibiotics may be needed to treat a noncompliant patient.
What I Learned from Writing this Article
I went into this thinking there was absolutely no validity to the blood type diet. If you read the Wikipedia article, or any of the abbreviated descriptions not on Dr. d’Adamo’s website, you get a short, biased description of the diet giving Dr. d’Adamo a bad rap. I tried my best to put my bias aside and was able to learn a few things about the following:
- Lectins: Eating Right 4 Your Type is geared toward more of a mainstream audience, but d’Adamo’s medical texts are much more technical and contain a lot of useful information. I learned a lot about lectins and their classifications. I also learned a lot about their corresponding carbohydrates and their binding mechanisms. I’ll definitely reference this material in future research
- ABO blood group risk factors: A lot more risk factors are associated with the ABO blood group than I knew about. I had only been aware of a few before, and I thought that the connection was somewhat novel. Now I can see how such a minor detail as having a tiny carbohydrate attached (or not attached) to the cell membrane can have an effect on one’s general health.
- Viruses: I learned a lot about viruses and their working mechanisms. The association between blood group and infection led me down a research trail into how specific viruses enter the cell and replicate.
- Theory: A lot of new theories and possibilities were opened up to me. Although there is not yet enough evidence for me to believe the theories I came across, I am now open to the possibility of many being legitimate. I am hopeful that new research will arise to study these theories deeper.
Optimism vs. Skepticism
It is important to maintain a healthy balance between optimism and skepticism. We need imaginative people to create new theories and ideas, as much as we need people to doubt these ideas and ask for proof. While I agree with Dr. d’Adamo in many areas, I think the biggest philosophical difference between the two of us is that he is more on the optimistic side of the spectrum, whereas I am more skeptical.
When I looked at his claims, I asked myself: Based on the data that I am given, what is more likely to be true? In many instances, there just wasn’t enough data to justify the diet. In summary, Dr. d’Adamo gets a lot of things right, but he has some things he needs to prove. Here is my breakdown:
 What Does the Blood Type Diet Get Right?
What Does the Blood Type Diet Get Right?
- Individualized nutrition is important.
- Lectins can damage our health, and we should work to mitigate that damage.
- There are health differences among people from different ABO blood groups.
- People shouldn’t eat candy bars, potato chips, or other junk food items.
- People should eat a whole food diet
- It is important for each person to be the primary advocate for their own personal health.
What Does the Blood Type Diet Need to Prove?
- We need to see specific in vitro research on the proposed mechanisms of lectins and blood group–specific glycosylation
- We need to see some broader, in vivo research done on controlled populations.
- The lectin biochemistry needs to be looked at again and corrected. Many of the foods appear to be miscategorized
- The errors in the biophysics need to be corrected and the pertaining sections need to be revised or removed.
- The evolutionary biology needs to have a stronger scientific connection, or it should be revised or removed.
- The mechanics of digestion and metabolism need to be clearly understood and appropriately described.
- Epigenetic factors need to be considered and accounted for.
Conclusion
 Scientific discourse is essential for advancement. When you disagree with someone’s ideas, you need to ask yourself:
Scientific discourse is essential for advancement. When you disagree with someone’s ideas, you need to ask yourself:
- “What would it take to change my mind?”
- “Am I completely closeminded?”
- “If stronger evidence was presented, could I change my belief?
There are a lot of great things about the blood type diet. It is far superior to the Standard American Diet (SAD), but it makes some claims that need more scientific support. Unfortunately, I think that most people don’t dig deep enough into Dr. d’Adamo’s writings. They oversimplify his work, and they dismiss his ideas. With this type of attitude, we will never know whether his ideas have substance, because it deters researchers from being open-minded enough to put some real effort into it.
After reviewing all the material, it would be crazy to say that there are no lectins in foods that are blood group specific. We know that there are blood group–specific viruses, so why wouldn’t there be blood group–specific foods? With proper research, we might find some of them. They could be as Dr. d’Adamo proposes, or they could be completely different. Some lectins may not have any greater or lesser impact on a specific blood group—just like most viruses don’t—but we will never know until we look.
Ultimately, we need to base our beliefs on what is observable, actionable, and repeatable. For me, there is not enough observable evidence of effectiveness to support the blood type diet. For those who are more on the optimistic side of the spectrum and wish to try something new, they could do a lot worse than the blood type diet, that’s for sure! However, in my opinion there is more value in choosing foods to optimize the gut bacteria, ensuring a healthy digestive system. It’s better to design your diet around your individual microbiome rather than on your particular blood group.
Thanks for reading! I would love to hear your comments on the Fix Your Gut forum!
- https://www.vegsoc.org/ ↩
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3499995/ ↩
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1273254/ ↩
- http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0084749 ↩
- http://ajcn.nutrition.org/content/98/1/99.long ↩
- https://www.amazon.com/China-Study-Comprehensive-Nutrition-Implications/dp/1932100660/ ↩
- https://pdfs.semanticscholar.org/f5e8/258d4203e73b1507369038eff3b3ff5714d9.pdf ↩
- http://biologiaevolutiva.org/jbertranpetit/wp-content/uploads/2014/11/JB2008-274-Calafell-HumGen.pdf ↩
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1831834/ ↩
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4800640/ ↩
- http://www.jmrps.net/eJournals/_eJournals/1_ORIGINAL%20ARTICLE.pdf ↩
- http://onlinelibrary.wiley.com/wol1/doi/10.2903/j.efsa.2008.726/abstract ↩
- https://www.ncbi.nlm.nih.gov/pubmed/7657599 ↩
- https://www.ncbi.nlm.nih.gov/pubmed/3288622 ↩
- https://www.ncbi.nlm.nih.gov/pubmed/3288622 ↩
- https://link.springer.com/article/10.1023/A%3A1006976129458 ↩
- https://www.ncbi.nlm.nih.gov/pubmed/21536757 ↩
- https://link.springer.com/article/10.1007%2FBF01675194 ↩
- http://onlinelibrary.wiley.com/doi/10.1002/cne.902680202/abstract ↩
- http://onlinelibrary.wiley.com/doi/10.1002/cne.902680202/abstract ↩
- https://www.ncbi.nlm.nih.gov/pubmed/11030554 ↩
- https://www.ncbi.nlm.nih.gov/pubmed/10647178 ↩
- https://link.springer.com/article/10.1007/s00425-006-0467-x ↩
- https://academic.oup.com/glycob/article/14/12/1247/763406/A-database-analysis-of-jacalin-like-lectins ↩
- http://gut.bmj.com/content/27/12/1457.short ↩
- Danisco Health & Nutrition ↩
- https://bmcmicrobiol.biomedcentral.com/submission-guidelines/peer-review-policy ↩
- https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-016-3290-1 ↩
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3190290/ ↩
- https://www.ncbi.nlm.nih.gov/pubmed/20937632 ↩
- http://onlinelibrary.wiley.com/doi/10.1111/j.1541-4337.2011.00164.x/pdf ↩
- http://onlinelibrary.wiley.com/doi/10.1111/j.1541-4337.2011.00164.x/pdf ↩
- http://onlinelibrary.wiley.com/doi/10.1002/mnfr.200700002/full ↩
- https://www.ncbi.nlm.nih.gov/pubmed/10872230 ↩
- https://www.ncbi.nlm.nih.gov/pubmed/24656332 ↩
- https://www.ncbi.nlm.nih.gov/pubmed/10872230 ↩
- https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/aje/172/11/10.1093/aje/kwq299/2/kwq299.pdf?Expires=1498062038&Signature=EerEWXiyVPql05KmrgLYFe8ZKfuv6TbDQKzK5bBzd-2hdw~2eAtzEU2j6Z92AmAYIObB9FucvI3qO-jsBVTn5wucF~RJpJ7BZ2vqUKjOxKF-k60MBLUyO-u7oHhmVD7XCQgcNMKa3niEaYluBI8OVpuYT5Tri4h8mokyMHZqOLJF~7Z2iUmwau8k01TY2KiALCsc26Tz9y3wiaaAbg1SF3~29MAJDftL7hlqlcDS7rJtrkLQ-Q47U1UwoRUgpoodX0muoSUJ3i-https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/aje/172/11/10.1093/aje/kwq299/2/kwq299.pdf?Expires=1498062038&Signature=EerEWXiyVPql05KmrgLYFe8ZKfuv6TbDQKzK5bBzd-2hdw~2eAtzEU2j6Z92AmAYIObB9FucvI3qO-jsBVTn5wucF~RJpJ7BZ2vqUKjOxKF-k60MBLUyO-u7oHhmVD7XCQgcNMKa3niEaYluBI8OVpuYT5Tri4h8mokyMHZqOLJF~7Z2iUmwau8k01TY2KiALCsc26Tz9y3wiaaAbg1SF3~29MAJDftL7hlqlcDS7rJtrkLQ-Q47U1UwoRUgpoodX0muoSUJ3i-fCEbPppJ2k823LUthmKAofOaoRICUlkrr0UsrgOFA-SidxgeMzne0zgRVwwtW~lGNeHAZaGOhdA__&Key-Pair-Id=APKAIUCZBIA4LVPAVW3Q ↩
- https://www.ncbi.nlm.nih.gov/pubmed/20937632 ↩
- http://www.amjmed.com/article/0002-9343(59)90345-6/abstract ↩
- https://www.ncbi.nlm.nih.gov/gene/1950 ↩
- https://www.ncbi.nlm.nih.gov/pubmed/1582810 ↩
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1117475/ ↩





Thank you so much for this! I, too, had taken too much organic chemistry–and am too “stuffy” –to take the blood type diet seriously…even more so because I am a Type B who appears to thrive on wheat. But after recently learning that blood type is well known to differentially affect immunity to several viral diseases, I wondered if I had dismissed the theory too easily.
So thank you for taking the whole hypothesis seriously enough to unpackage various aspects which are reasonable, plausible, hopelessly outdated, or just contrary to well-supported research.
I remain somewhat confused by the lectin controversy, since I do know people whose healthy vegetarian diets do not seem to agree with them, yet I don’t seem to have digestive issues regardless of what I eat. So it was fascinating to hear that wheat sensitivity can affect the muscles and the eyes, rather than just the digestion.
I may have to watch more closely and reconsider my conviction that I must be one of the lucky ones with a sturdy GI tract that is not affected by any of these insidious plant proteins.
Considering how following a blood type diet for myself has 110% pinpointed a “wicked reaction” (dr’s-Allergist etc) and avoiding lectins for my blood type is A MUST FOR MYSELF TO EAT DAILY, I highly also ” question” a chemist’s opinion who’s ” been tapped by prominent supplement companies” from your own website, I also question his motives So, how do we “know our individual microbiology”.. Buy your e-book?, or buy your coaching?.,,yes I’ve also read and used all of the same same sources of information and references you’ve listed on your website. I agree with you mrfixyourgut.com too but I also see and hear the same between the lines scenerio also. Why doesn’t your site mention anything, being an organic chemistry background?, even mention lectins along with GMO’s and the reason we have these “super grains” and ahh super lectins..wheat, potato, kidney beans, corn, tomato..? If two cents of one’s own opinion is allowed here: Nutritionists..and no, insurance doesn’t cover because it works. They also have Ph.D’s and Masters as well. No two human bodies nor their individual chemistry is the same.
I read this article with great interest, since I’m Blood Type O and Dr. D’Adamo’s diet says I should avoid wonderful foods such as avocados, cabbage in all forms (sauerkraut is supposed to be so healthy for the GI), and an herb that is one of the main ingredients in Essiac, a cancer-fighting formula that has documented proven results over the years. (and I’m dealing with cancer).At one point he said Spirulina was also on the NO list, but then changed his mind later. It’s hard to find out why he’s put these foods on the NO list, one has to assume it has something to do with lectins. There’s a part of me that just doesn’t want to accept his theories anymore and eat the above foods, plus other ones on the NO list that are generally considered to be healthy.
However, it’s true for me that I am also gluten intolerant, allergic to dairy, and don’t do well with citrus (except for lemon), which he also describes as type O traits, and I also avoid grains (better for my GI and also less sugar, which I minimize), so there is some accuracy in some of his classifications for me—probably also due to my family genetics, and the state of my gut. And vegetarian diets don’t give me enough energy…I do much better on a general Paleo style diet. So I’m leaning towards more flexibility these days, and see how I feel, rather than following his diet as exactly as I’ve been doing. Comments welcome.
I followed the BTD when it first came out, because I had been struggling with arthritis. Three months later I was pain free, so literally became a fan. The explanation for the different blood types is just theory, we don’t know why or how they came about. Some of the early food values were theory also, and many were upset because they thought the changes of food values were errors in the next book. he explained to us that ti was an evolving science so tings were going to change over time. I attended two of his conferences, became an IFHI master, then stopped when his science evolved to Genotyping, because it was just getting too complicated. If I cared to fine tune my diet, I would probably go to one of his clinics to be Genotyoed, but I just don’t wanna. I’m 62, need no medications, in good shape for my age. What I want to say to you is this, if you want to eat avocado because you like it, eat it. Just don’t eat it every day because someone convinced you it is so good for you, where is their science? In fact, look for the science for his food values, see if they hold water, and whatever you do, enjoy!
I greatly appreciate this article and the obvious care and attempts at open mindedness you put into it.
In theory, I agree with everything you state.
In practice I have seen into the 100’s of cases where people who were already eating a healthy, little to no junk food diet, improved greatly when they began eating “right for their type”. Improvements were measurable, from reduction in pain and need for pain medication to vastly improved heart, rheumatoid, etc diagnostic test reports.
So while there are plenty of holes in the theory, and certainly nothing is for everyone, my bottom line is that even while I do not believe in it I keep seeing it work.
That’s a really great article, thank you for putting so much work into explaining the chemistry behind the facts.
Type A phenotype has the N-acetylgalactosamin ontop Fucose to form the A-Antigen, not N-acetylglucosamine. This NAGlucosamine is ubiquitous in all blood types in various tissues and lectins attaching to NAG will cause problems for everyone.
thank you, it is all i needed to know just right now!